What is the Nutrition Care Process?
The Nutrition Care Process (NCP) is a systematic framework that is designed to guide dietitians in providing high-quality, individualized nutrition care to clients, whether individuals, families, or populations. It uses the best available evidence to make decisions while taking the client's needs and values into consideration. The NCP was created by the American Dietetic Association (ADA), now known as the Academy of Nutrition and Dietetics (AND), in 2002.1,2,3
The Nutrition Care Process Model (NCPM) (Figure 1) is a visualization of the workflow of dietetic professionals and the steps namely: nutrition assessment, nutrition diagnosis, nutrition intervention, and nutrition monitoring and evaluation. The NCPM also shows the internal and external factors that impact the application of the NCP.1,4
Figure 1. The Nutrition Care Process Model as adapted from the Nutrition Care Process and Model Part I (2008).5
The Nutrition Care Process Terminology (NCPT) is used in conjunction with NCP. It is a standardized language for nutrition and dietetics used to document nutrition care. It aims to provide a glossary of terms, codes, and definitions specific to dietetic practice.3 Dietitians around the world use the NCP and NCPT to maintain the consistency and clarity of dietetics-related healthcare records, as well as to collect and analyze patient outcomes.6 Furthermore, regular use of the NCP by dietitians in patient treatment demonstrates improved positive patient outcomes.10
What are the steps of the NCP and the specific roles of RNDs?
The four steps of the nutrition care process described above are unique but interconnected. The steps are not sequential, and the process cycles through nutrition assessment, nutrition diagnosis, nutrition intervention, and nutrition monitoring and evaluation until the nutrition goals are accomplished. The process may involve one or more cycles.7 To make it unique and exclusive to the dietetics profession, the word nutrition is inserted before each phase of the process.
To achieve a positive client health and nutrition outcome, the RND must apply critical thinking and evidence-based nutrition care to every step of the NCP. Below are the steps and the corresponding roles of RNDs:
First Step: Nutrition Assessment
The first step is an ongoing and dynamic process that involves the collection, reviewing, clustering, interpreting, and synthesizing pertinent data that is used to identify the client's nutrition-related problems, if any, and their causes. In this step, the client's status is continuously reassessed and analyzed, and nutrition assessment data or indicators are compared to established guidelines, recommendations, and/or objectives.8,9
The RND's role here is to gather relevant information about the client's food and nutrition history, anthropometric measurements, biochemical data, medical tests and procedures, nutrition-focused physical findings, and a client history. Medical charts, caregiver and family interviews, observation and measurement, the client's interview, and health care providers' interviews can all yield this information. Surveys and epidemiological studies can be used to gather relevant data for population groups. The data collected by the RND in this step is used in the next step of the NCP, which is the nutrition diagnosis.2,7, 8,9
Second Step: Nutrition Diagnosis
To treat an existing nutrition problem or problems, the dietetic practitioner must first identify and label them.8 A nutrition problem may be present at the moment or could develop in the future. This step connects the first and second NCP steps. This step requires careful consideration because a medical diagnosis is not the same as a nutrition diagnosis.2 A medical diagnosis is characterized as a disease or pathology of a particular organ or body system that is treatable or preventable. It will remain unchanged as long as the disease condition exists. On the other hand, nutrition diagnosis varies according to how the patient, client, or group reacts.7
Using the pertinent information gathered in the NCP's first step as a foundation and guide, the RND determines the proper nutrition diagnosis or diagnoses in this phase. The PES (Problem, Etiology, Signs, and Symptoms) statement is used to write the nutrition diagnosis. It describes each nutrition problem, its underlying causes, and the evaluation results that support the diagnosis. When drafting the nutrition diagnosis, the RND consults the NCPT7,10
Third Step: Nutrition Intervention
To address or at least improve the identified nutrition problem or problems, the third step of the NCP involves deliberate planning and designing of actions aimed at modifying the client's nutrition-related behavior, risk factor, environmental condition, or aspect of health status. Nutrition interventions are customized to meet the specific needs of each client based on the nutrition diagnosis and its etiology. 7,11
The role of the RND in this step is to select appropriate evidence-based and up-to-date interventions tailored to the client’s needs to address the nutrition diagnosis, targeting directly the root cause of the nutrition problem and aimed at alleviating the signs and symptoms of the diagnosis.7,11
Fourth Step: Nutrition Monitoring and Evaluation
At this stage, the dietitian's job is to assess the client's progress in fixing and improving the nutrition problem or problems, as well as whether the goals or outcomes of the nutrition intervention are being met. Finding the results or indicators that are relevant to the nutrition diagnosis, as well as the strategies and objectives of the nutrition intervention, is the task of this step. Along with these tasks, it involves evaluating the client's progress by comparing it to past performance, intervention goals, or reference standards, as well as reviewing and measuring the client's status at a prearranged follow-up. As the reassessment is being done, this step refers back to the initial step.7,12
The RND tracks how the nutrition intervention chosen in the previous step is affecting the resolution of the nutrition diagnosis or diagnoses in this step, supplying proof of the intervention's efficacy or ineffectiveness in modifying the client's condition. The RND then compares the current status of the client with his or her previous status, the nutrition intervention goals, reference standards, and evaluates the overall impact of the nutrition intervention on the client’s nutrition diagnosis(es) and health outcomes.7,12
What are the current guidelines for the NCP in the Philippines?
Republic Act No. 10862, also known as the Nutrition and Dietetics Law of 2016, was enacted in 2016 to regulate and standardize the practice of nutrition and dietetics in the Philippines. One of the scopes of practice of the RNDs under this law’s Article VI, Section 26, is providing medical nutrition therapy (MNT) through the application of the nutrition care process for disease prevention, treatment, and management.13
The Philippines' Department of Health (DOH) Administrative Order No. 2019-0033: Guidelines for the Implementation of Nutrition Care Process in Hospitals was enacted on August 28, 2019, in recognition of the significance of the Nutrition Care Process (NCP) in the provision of nutrition care. The order's main goal is to provide guidelines for the implementation of the NCP in public and private hospitals, giving them the authority and guidance to operationalize and institutionalize the NCP in their respective establishments. According to the directive, all hospitals, regardless of level (1, 2, or 3), ownership (private or government), or service capability (general or specialty), must implement NCP. The order outlines the precise duties and responsibilities of each member as well as broad and detailed guidance for how the NCP must be implemented in hospitals.14
The nutrition care algorithm (Figure 2) below outlines how to put the NCP into action. All admitted patients must undergo a nutrition screening by a registered nurse prior to implementation in order to identify patients who are nutritionally at-risk, including those who are critically ill. Once identified, the physician on duty must refer the patient needing medical nutrition therapy to the RND.
The RND then must accommodate all referrals within 24-48 hours after admission and must initiate nutrition assessment to categorize patients based on the following risk criteria:
- High-risk patients or those with severe malnutrition who have a “high risk” of developing malnutrition and nutrition-related complications;
- Moderate-risk patients or those who have a “moderate risk” of developing malnutrition and nutrition-related complications; and
- Low-risk patients or those admitted for more than 15 days.
Patients in the high-risk category must receive nutrition care within 24 hours. While those identified as low-risk must be reassessed.
Nutrition assessment must be the RND's starting point in developing and implementing a nutrition care plan. The identification of a nutrition diagnosis or diagnoses is the next step, and it is based on the data evaluation from the previous step. After that, the RND will create nutrition interventions, such as meal plans and prescription diets. This must be confirmed with the attending physician. The RND is responsible for carrying out the nutrition intervention plan once it has been agreed upon. Following that, the RND will keep an eye on developments and assess how well the objectives or intended results of the nutrition intervention are being achieved. The RND must record each step of the NCP in the patient's chart.14
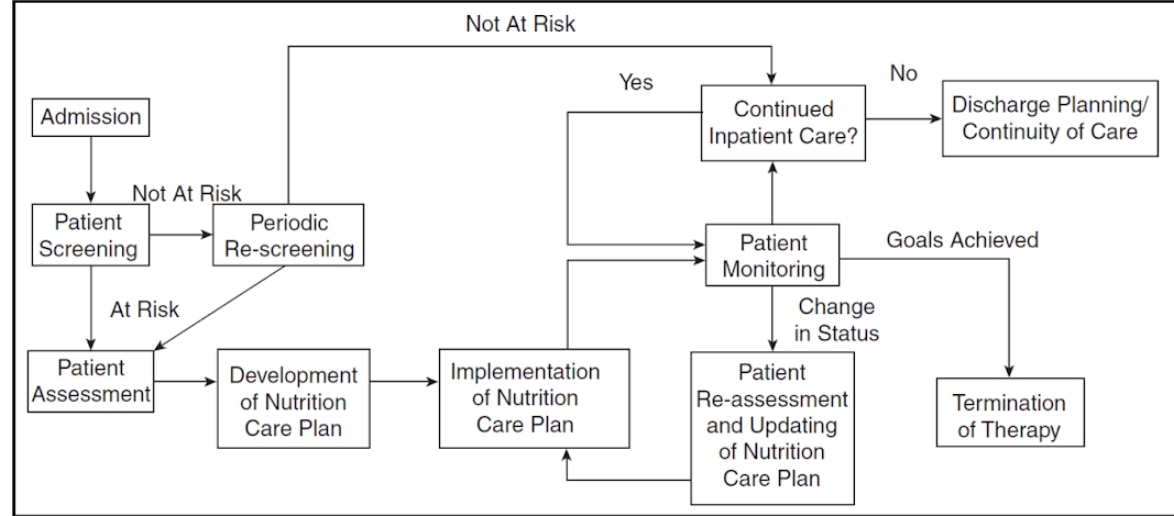
Figure 2. Nutrition Care Algorithm (Adapted from Standards for Specialized Nutrition Support: Adult Hospitalized Patients by Ukleja A, et al.; 2010).14
What improvements can be made in the practice of NCP in the Philippines?
A study titled “Ascertainment of Nutrition Care Process (NCP) Implementation and Use of NCP Terminologies (NCPT) among Hospital Dietitians in the Philippines”, showed that most hospital dietitians had a high level of knowledge on NCP and NCPT (92.3%, n = 65) and positively perceived their implementation (84.6%, n = 65). However, only 60% (n = 65) of them had a high level of NCP practice.15
The identified facilitators of implementation were:
- Collaboration, dedication, and commitment of the healthcare team;
- Institutionalization of NCP laws and policies;
- Budget allocation for NCP-related activities;
- Monitoring and consistency of NCP implementation; and
- work schedule.15
On the other hand, the identified barriers to NCP implementation were:
- insufficient resources, specifically lack of important equipment such as hospital bed scale, insufficient staff nurse and dietitian, and insufficient hospital budget;
- Lack of orientation, training, and support for the healthcare staff;
- Organizational and administrative constraints such as lack of communication among members of the healthcare team, absence of an established nutrition support team, and the cost of the nutrition care package;
- Pandemic constraints;
- Insufficient time to implement and document NCP due to understaffing; and
- Lack of confidence to conduct NCP due to perceived lack of NCP training. 15
The practice of NCP may be improved with the help of the stakeholders themselves. Healthcare teams can ensure proper implementation and communication of the NCP. The hospital institution can provide the necessary logistics and management support and ensure strict compliance with the implementation of AO No. 2019-0033. Government agencies can do their part by overseeing and ensuring the implementation of the order and compliance of RNDs with RA No. 10862. Finally, professional organizations can offer available training on NCP to help improve the confidence and expertise of RNDs to conduct NCP. Focusing on how to address the barriers to NCP implementation and strengthening the facilitators of its implementation will help improve the practice of NCP in the Philippines.
Tip: Ensure thorough documentation of the NCP and communicate to the healthcare team.
It should be stressed that documentation is a crucial on-going process that must be done in all steps of the NCP. Proper and complete documentation is important, as the client’s chart is used to communicate the NCP to other members of the healthcare team.
The information to be recorded in the client’s chart must be relevant, accurate, and timely, and must use the standardized language of NCPT.7 The date and time that each step of the NCP is conducted must be documented.
The nutrition assessment documentation must include pertinent data collected and compared with standards, information on the client’s perceptions, values, and motivations in relation to the presenting nutrition problems, changes in the client’s level of understanding, food-related behaviors, and other clinical outcomes for appropriate follow-up, and the reason for discontinuation of NCP implementation. 7
Nutrition diagnosis documentation must be properly written following the PES statement and must be constantly updated depending on new data available. 7,10 Each nutrition diagnosis must be labeled, whether new, active, resolved, or discontinued, to communicate its status with the other members of the healthcare team.16
With regards to the nutrition intervention, documentation must include the specific treatment goals and expected outcomes; recommended interventions tailored to the client’s needs; any adjustments to the plan and justifications; the client’s receptivity; referrals made and resources used; other relevant information in providing care and monitoring progress over time; plans for follow-up and frequency of care; and the rationale for discharge, if appropriate.7
Last but not the least, documentation of nutrition monitoring and evaluation must include specific indicators measured and results; progress toward goals; factors facilitating or hampering progress; other positive or negative outcomes; and future plans for nutrition care, monitoring, and follow-up or discharge.7
Conclusion
It is essential to adhere to a standardized NCP when providing nutrition care to clients because it supports the adoption of evidence-based nutrition care, which improves patient outcomes. Standardized NCP and NCPT use also results in more thorough and better documentation of nutrition care and client outcomes, which promotes better teamwork and communication. Therefore, when providing high-quality and comprehensive nutrition care, RNDs must use the standardized NCP and NCPT.
In the Philippines, NCP and NCPT implementation by the hospital RNDs may be improved with further support from the healthcare team, the hospital, government agencies, and professional organizations, to

 Joan Delomen , RND, MSc
Joan Delomen , RND, MSc















No comments here yet.