The Anatomy of the Kidney: What is it made of?
The human kidneys are small, fist-shaped (around 11-12 cm long, 6 cm wide, and 3 cm thick) organs symmetrically located in the lower back, from the T12 to the L3 vertebrae.1 Each kidney has a cortex, the outer region, and a medulla which is the inner region that is divided into renal pyramids. There is also the so-called functional unit of the kidney, the nephron, and there are approximately 1 million of it in a single kidney.2
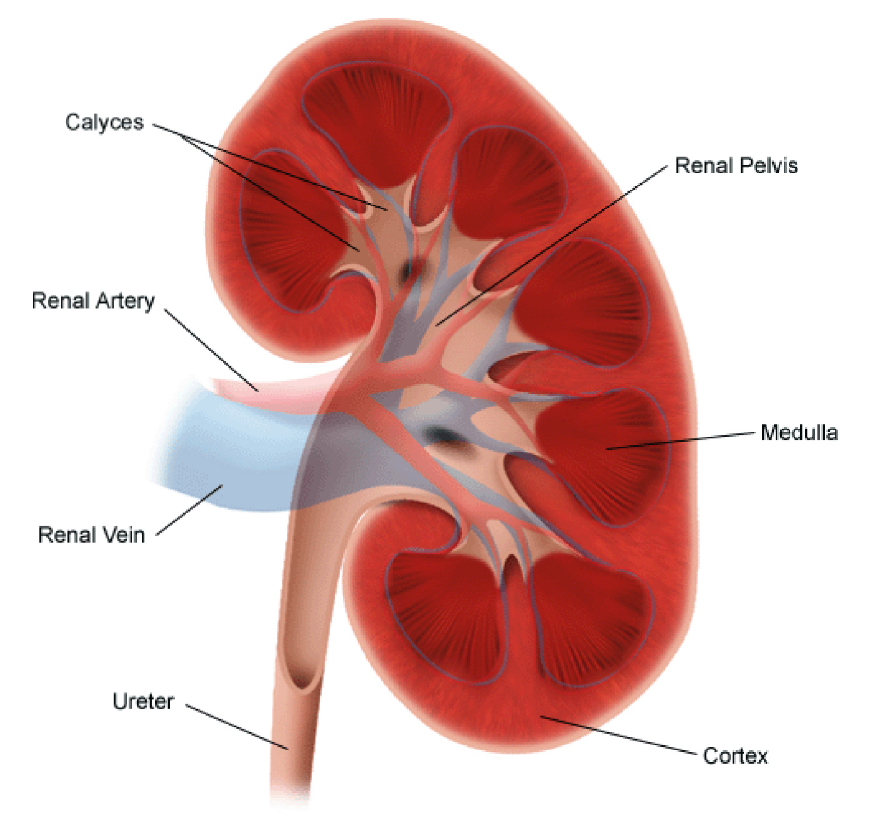
Figure 1. Anatomy of the Kidney (Stanford Children’s Health, n.d.)
Kidney at Work: When it is functional and not functional
The kidneys have many functions, and these are some:
- Excretory or removal of waste products from the body through urine
- Acid-base balance through a buffer system that maintains blood pH at around 7.4
- Endocrine synthesis of hormones such as renin, erythropoietin, and active Vitamin D3 (calcitriol)
- Fluid and electrolyte balance
The size of human kidneys may be small, yet it constitutes a powerful engine that can process about a cup of blood every two minutes.3
Question: What happens if there is a decline in kidney function?
Renal failure does not usually come with warnings and may be sudden, thereby causing Acute Renal Failure (ARF). The good news is patients with ARF may still recover with Medical Nutrition Therapy (MNT). However, when ARF goes untreated or unmanaged, it can progress to Chronic Kidney Disease (CKD).
Chronic Kidney Disease is the condition in which a patient’s kidneys stop working at its optimal capacity, usually due to glomerular disease (e.g., glomerulonephritis), hypertension, or diabetes (diabetic nephropathy). This means failure to filter waste from the blood and leading to a waste build-up in the body. CKD usually doesn’t have early signs, and this might mean patients usually know about their condition at the advanced stage.
According to the National Kidney and Transplant Institute,4 while CKD is usually asymptomatic, it can present with high blood pressure, edema, easy fatigability, nausea and vomiting, and loss of appetite. CKD can be functional or structural in origin. In the elderly (ages 60 and above), loss of kidney function may come naturally, therefore dietary adjustments should be made to prevent further decline. In the Philippines, where the cases of CKD are rising, the main cause of CKD is diabetes.5
CKD is classified based on the cause which is either: the Glomerular Filtration Rate (GFR) category or the albuminuria (abnormal loss of albumin through the urine) category.
Glomerular Filtration Rate, which is the amount of filtrate formed per minute based on the total number of functioning glomeruli, can be calculated using the following equation6:
Need to Know: Prognosis, stages, and what it means
The status of CKD can then be prognosticated using GFR, albuminuria category, and cause of CKD based on this chart:
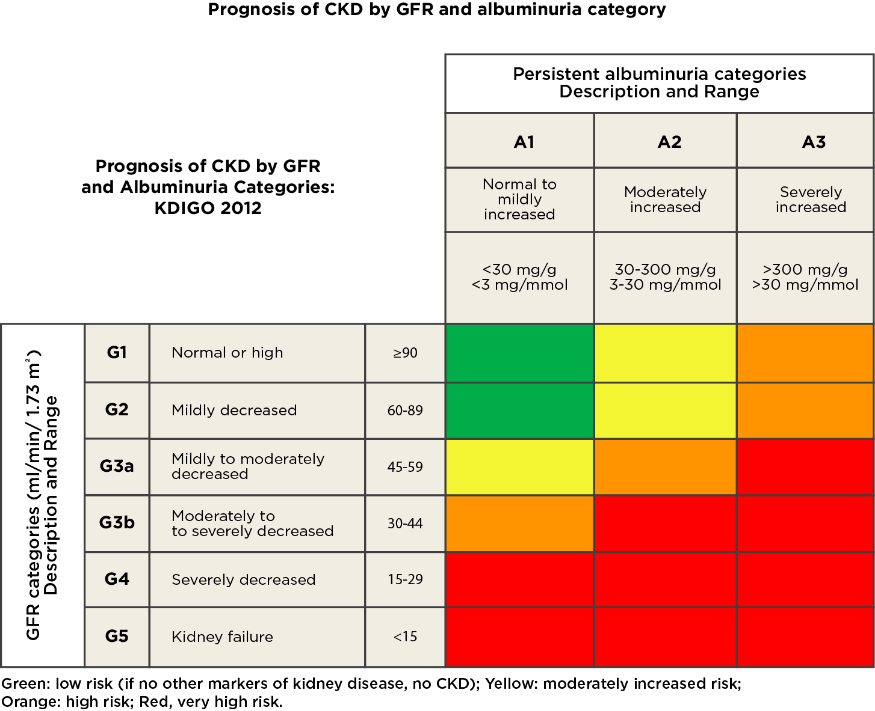
Figure 2. Prognosis of Chronic Kidney Failure and Albuminuria Category (KDIGO, 2012)
The stages and treatment modalities are further articulated by the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF-K/DOQI) guidelines:
Table 1. Stages of Chronic Kidney Disease: A Clinical Action Plan (NKF-K/DOQI, n.d.)
| Stage | Description | GFR | Action (includes actions from preceding stages) |
|---|---|---|---|
| 1 | At increased risk kidney damage with normal or increased GFR | >90 with CKD risk factors > 90 | Screening, CKD risk reduction diagnosis and treatment. Treatment or comorbid |
| 2 | Mid decrease in GFR | 60 to 89 (may ne normal for age) | Estimating progression |
| 3 | Moderate decrease in GFR | 30 to 59 | Evaluating and treating complications |
| 4 | Severe decrease in GFR | 15 to 29 | Preparation for kidney transplant therapy |
| 5 | Kidney Failure | <15 or dialysis | Replacement, if uremia is present |
For the elderly (60 years and above), decreased GFR (Stages 1 to 2) may be present, and this is normal. In both elderly and non-elderly patients with CKD up to Stage 3 GFR, MNT may be used as an intervention, to prevent further worsening of the condition.
Generally, during GFR Stages 1-4 the treatment plan is to screen for and manage cardiovascular disease. Moreover, care providers should design the treatment to prevent diabetes, hypertension, and dyslipidemia as much as possible. If these are already present, they should be managed.
Specific to GFR Stage 2, management still involves reducing risks of cardiovascular disease, but more importantly at this stage, the care providers must monitor loss of kidney function more closely. This way, the said care providers can decide if the patient will eventually need to be put on renal replacement therapy (e.g., dialysis or kidney transplant).
Most CKD-related complications start at GFR Stage 3; thus, care providers must treat complications as they come. Upon detection of complications, they are treated alongside the CKD through a variety of methods. Anemia and secondary hyperparathyroidism are two common complications that may arise at this stage.
If the patient with CKD is at GFR Stage 4, patient education on dialysis and kidney transplant must be started. This is the stage during which the patient is prepared for either dialysis or kidney transplant. Options are made available based on many factors, including preference of the patient, comorbidities, and family support. Moreover, kidney transplantation is indicated once the patient is assessed further.
During GFR Stage 5, there is kidney failure and renal replacement therapy is initiated at this stage. Kidney transplant candidates have better outcomes than those receiving dialysis treatments.9
The Role of Nutrition: Some General Knowledge
Medical Nutrition Therapy (MNT) is among the primary and early treatments for CKD. MNT aims to maintain the quality of life at the highest level, minimize secondary effects of CKD, slow the CKD progression, and delay the need for dialysis. For patients waiting for kidney transplants (pre-transplant), MNT ensures optimal health until transplantation has been performed, and MNT may continue to the post-transplant stage. This points out that MNT is crucial and encompasses the CKD spectrum.
There are three types of diets depending on the status of the patient:
- Pre-Dialysis Diet
- Dialysis Diet – also known as Renal Replacement Therapy or RRT
- Organ Transplantation Diet
Renal Diet Assessment: Into the Specifics
MNT for a patient with CKD is highly specific. This is to make sure that, given the CKD grade, the kidney can still work at its best. Done right, a good diet might prevent CKD from worsening, and it is best to work closely with the doctor and RND for proper guidance. Once a patient gets diagnosed, the RND can already start working on the renal diet. The RND can then start building from the urinalysis results of the patients and include assessing others, such as BMI and other anthropometric measurements.
Table 2. Renal Diet Assessment
| RENAL DIET ASSESSMENT | |
|---|---|
| Anthropometric Assessment |
|
| Biochemical Assessment |
|
| Clinical Assessment |
|
| Dietary Assessment |
|
Breakdown of Nutrients: Essentials and their Match
As mentioned, MNT is highly specific for patients with CKD as it involves the modification of certain nutrient intakes to adjust to the existing health of the kidneys.
The following table contains general recommendations for RNDs to start building diets for patients with CKD. In this table are protein, sodium, potassium, and phosphorus, the four most important nutrients to be observed in patients with CKD.
Usually, patients with CKD are prescribed a low-protein diet since protein may add stress to the kidney while sodium affects water retention and may promote swelling, which can also make the kidneys work harder.
The kidney, as mentioned earlier in this article, maintains electrolyte balance, and potassium is among the electrolytes that need to be balanced. Excessive or low levels of potassium may cause muscle cramps, problems with the heartbeat, and muscle weakness, among others.
Phosphorus is another nutrient that is regulated by the kidney. Dysregulated phosphorus may lead to the resorption of calcium from the bones, and this may turn the bones brittle. Phosphorus and potassium take more focus on patients on dialysis.
Table 3. Nutrient considerations for Medical Nutrition Therapy of Chronic Kidney Disease patients (Rolfes, 2018)
| NUTRIENT | PREDIALYSIS | HEMODIALYSIS | PERITONEAL DIALYSIS |
|---|---|---|---|
| Energy (kcal/kg body weight) | 35 for <60 years old 30-35 for ≥60 years old | 35 for <60 years old 30-35 for ≥60 years old | 35 for <60 years old 30-35 for ≥60 years old (total kcalories should include those absorbed from the dialysate) |
| Protein (g/kg body weight) | 0.60-0.75 (≥ 50% high-quality proteins) | ≥1.2-1.3 (≥ 50% high-quality proteins) | ≥1.2-1.3 (≥50% high-quality proteins) |
| Fat | As necessary to maintain a healthy lipid profile | As necessary to maintain a healthy lipid profile | As necessary to maintain a healthy lipid profile |
| Fluid (mL/day) | Unrestricted if urine output is normal | 1000 plus urine output | As necessary to maintain fluid balance |
| Sodium (mg/day) | 1000-3000 | 1000-3000 | 2000-4000 |
| Potassium (mg/day) | TABLE 3. Nutrient considerations for Medical Nutrition Therapy of Chronic Kidney Disease patients (Rolfes, 2018) Unrestricted unless hyperkalemia is present | 2000-3000; adjusted according to serum potassium levels | 3000-4000; adjusted according to serum potassium levels |
| Calcium (mg/day) | 1000-1500 | ≤2000 from diet and medications | ≤2000 from diet and medications |
| Phosphorus (mg/day) | 800-1000 if serum phosphorus or parathyroid hormone is elevated | 800-1000 if serum phosphorus or parathyroid hormone is elevated | 800-1000 if serum phosphorus or parathyroid hormone is elevated |
RNDs and doctors should not forget to remind patients about their daily fiber and water intake to take advantage of fiber’s weight loss and weight management properties. Preventing other complications, such as hypertension, obesity, and diabetes in patients already with CKD will prevent worsening of outcomes.
Nutrition Care Process: Everyone on Board
By following the Nutrition Care Process (NCP): Assessment, Diagnosis, Intervention, Monitoring, and Evaluation (ADIME), RNDs and doctors can prioritize the quality of life of patients concerning their ongoing treatment plans. With MNT, RNDs need to ensure that patients are on a healthy diet by eating in moderation and balancing nutritional intake. To ensure compliance and a patient's optimal quality of life, diet plans must also have variety.
An RND may also recommend keeping a food diary to improve monitoring once the CKD diet has started. Two important markers may be checked: serum albumin and normalized protein equivalent to nitrogen appearance (nPNA). Serum albumin can indicate the protein levels in the blood; if serum albumin is too low, there may be a low intake of protein, protein is being lost in the urine, or there might be an infection. On the other hand, nPNA indicates protein intake.11
Oral Nutritional Supplements
Protein-energy wasting (PEW) is a problem among patients on hemodialysis. According to the International Society of Renal Nutrition and Metabolism, PEW is a state of nutritional and metabolic derangements in CKD and end-stage renal disease (ESRD). It is characterized by muscle wasting and easily depleting energy stores, where both can lead to poorer outcomes and quality of life. The hypercatabolic state induced by uremia, anorexia due to low appetite, inflammation secondary systemic conditions (diabetes), and autoimmune conditions (that lead to CKD and ESRD) all contribute to PEW.
Due to this, there are Oral Nutritional Supplements (ONS) that are being used to feed patients and counteract PEW. ONS is fed to patients to supplement their main meals to reach the daily protein targets and other serum markers.
It should be noted that if a patient is still able to consume 75% of their dietary demands, there is no need for ONS. Consuming lower than 75% or 3/4 of their plate (around 60%-50%) necessitates ONS. Aside from oral means, other routes of supplementary nutrition are parenteral (delivery to the bloodstream) and enteral (delivery to the gut).
Points to Assess for Deciding Supplementary Nutrition12:
- Anthropometric Assessment
- Biochemical Results (e.g., creatinine level, etc.)
- Clinical Assessment (e.g., color, ambulation status, independence)
- Dietary Assessment
- Adequacy of food consumption (lower than 75%)
- 24-hour Food Recall
For better visualization, below is a sample case and set of computations for a 61-year-old patient in the pre-dialysis stage.
Table 4. Sample computation of renal diet prescription for pre-dialysis patients.
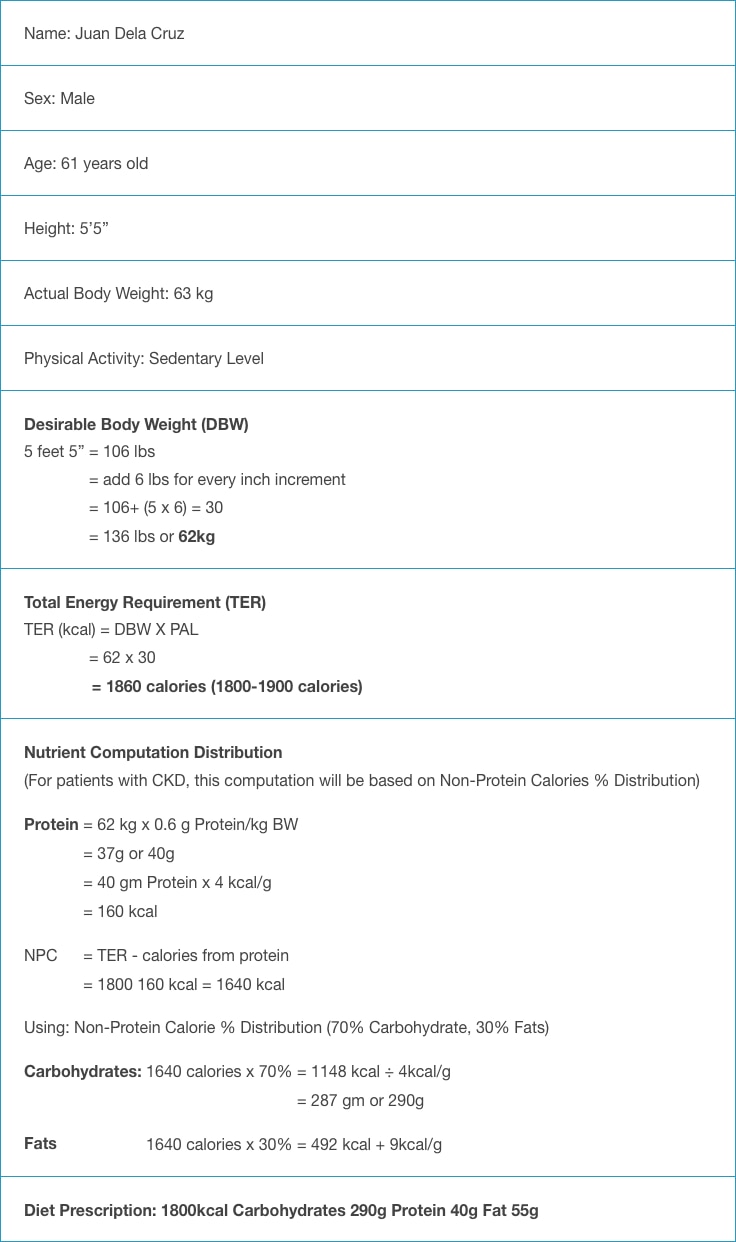
The prescribed diet for the patient is displayed below:
Table 5. Sample prescribed diet for pre-dialysis patients.
| PRESCRIBED DIET | |
|---|---|
Prescribed Diet: 1800 calories, 2000mg Sodium Low Protein Diet: Pre-dialysis | |
| FOOD ITEMS | NO. OF EXCHANGES/ SERVING PORTION | CARBOHYDRATES (g) | PROTEIN (g) | FATS (g) | ENERGY (kcal) |
|---|---|---|---|---|---|
| Vegetables | 2 exchanges 1 cup | 6 | 2 | - | 32 |
| Fruits | 2 servings | 20 | - | - | 80 |
| Milk | ½ serving 2 tablespoons Low fat | 6 | 4 | 2.5 | 63 |
Rice | 7 exchanges of medium protein (3 ½ cups rice) +
2.5 exchange of low protein (2 ½ slices bread) | 161
+ 57.5 218.5gm | 14
-
|
- |
950 |
| Meat, Fish, Eggs, Chicken | 2 ½ matchbox | - | 20 | 1.5 6 | 61.5 86 |
| Fats | 6-8 teaspoon/day | - | - | 40 | 360 |
| Sugar | 8 teaspoon/day | 40 | - | - | 160 |
| Salt | ¾ teaspoon/day | ||||
| Water | 6-8 glasses/day | ||||
| TOTAL | 290g | 40g | 50g | 1793 kcal |
Additional: Sodium (1009 mg), Potassium (1216 mg), Calcium (498 mg), Phosphorus (754 mg), Moisture content (737 mg)
Table 6. Sample three (3)-day renal diet menu plan.

In preparing a diet plan for patients with CKD, it is important to remember that foods can be substituted; uncommon foods may be replaced with native and indigenous foods. The key is to collaborate with the patient and take note of their preferences while being mindful of the available foods in their area. Recipe books may help, too, if it can make the patient follow instructions easier. These are all so that quality of life and adherence to the diet regimen is preserved.
Tips to Promote Kidney Health: Caring Goes A Long Way
Caring for the kidney comes with numerous guidelines, and it may be better to care for one’s renal health earlier rather than later. Below are tips to promote kidney health and avoid renal disease:
- Drink plenty of water daily (8 glasses for adults, 6-8 glasses for children).
- Maintain cleanliness & good hygiene.
- Make a habit of daily bowel movement.
- Do not delay urination
- Consult a doctor for any kind of throat & skin infection.
- Have a regular urinalysis (once to twice annually).
- Eat a balanced diet.
- Monitor blood pressure.
- Exercise daily.
- Follow complete vaccination and immunization.
- Do not smoke.
- Drink medicines as advised and prescribed by your doctor.
- Consult your doctor before taking any herbal supplements.
- For people with reduced kidney function, it is helpful to follow the correct & appropriate diet: modified protein, mild sodium restriction, and low cholesterol with adequate calorie and energy requirements
- Awareness and education (Dietary Instruction & Nutrition Counseling) are beneficial and helpful for patients’ diet compliance.
CKD may be difficult for the patient to manage, especially at the start. Therefore, it is important for the RND and doctors to provide support and education for the patient as they adjust to their new diet and lifestyle.
Kidney disease remains a leading cause of mortality in the Philippines13; moreover, it usually comes with comorbidities, such as cardiovascular disease and diabetes. As kidney function decreases, patients become more prone to other complications. In the end, CKD becomes a heavy burden not just for the patient but the family as well.
It is then important for those with risk factors to get tested regularly since CKD does not show early signs. Furthermore, the role of nutrition in preventing the progression of CKD should be recognized. Care providers should keep reminding at-risk patients that shifting to a healthier lifestyle early will always be more convenient, than having to adjust later.
Summary
Nutrition is an essential component in the management and treatment of the Chronic Kidney Diseases and malnutrition is a common problem and prevalent in dialysis patients. Medical Nutrition Therapy involves the modification of the following nutrients:
1. Protein
2. Sodium and Potassium Equilibrium
3. Calcium and Phosphorus Balance
4. Water and Fluid Intake
5. Vitamins and Minerals especially Vitamins B, C, D, and Iron.
Awareness and education referring to dietary instruction, nutrition counseling, and self-management of the patient are beneficial and helpful, preserving the quality of life.


 Socorro Balderamos , RND
Socorro Balderamos , RND














No comments here yet.