The Elderly

The United Nations defines the elderly as a person over 60 years old1 while conventionally, the term is coined for individuals having a chronological age of 65 years and older (or if a person is retired).
Unknown to some, there are three categories of elderly: the young old, the middle old, and the old-old. Those under the category of young old are 65-74 years old. Clustered under middle old are those with ages ranging from 75-84 years old. Lastly, those 85 years old and over are categorized as old-old.2
The age bracket may be slightly varied but one thing is commonly known: reaching that numeric feat entails a special kind of care and nutritional need that professionals and the general public must be mindful of.
Look Closer: Changes to Look Out For

Aging is linked to a variety of changes in the body which make it difficult for the elderly to meet their nutritional needs. Poor nutrition, on the other hand, increases the risk of malnutrition which would eventually cause a decline in the quality of life.
Apart from the changes, it is essential to look into the factors that make it a challenge to keep the elderly from eating nutritiously to be healthy. Understanding the context of patients will guide Nutritionist-Dietitians in formulating a plan and help create a better relationship with the client, one that will make it easier for patients to follow what is recommended to them.
Digging Deeper: Factors Affecting Nutrition in the Elderly
Aging is linked to a variety of changes in the body which make it difficult for the elderly to meet their nutritional needs. Poor nutrition, on the other hand, increases the risk of malnutrition which would eventually cause a decline in the quality of life.
Apart from the changes, it is essential to look into the factors that make it a challenge to keep the elderly from eating nutritiously to be healthy. Understanding the context of patients will guide Nutritionist-Dietitians in formulating a plan and help create a better relationship with the client, one that will make it easier for patients to follow what is recommended to them.
To start, here are 7 factors:
The Catch: A race against time
As age increases, so is the risk of sickness. The elderly, given their situation, are prone to nutrition-related problems. As RNDs, being mindful of these will help craft a better plan for patients.
Here are the common nutrition-related problems among the elderly:
- Diabetes mellitus - Around 13.8% of the Filipino elderly population had elevated fasting blood glucose levels. The youngest age group, 60-69 years old, had the largest percentage (15.3%) of people with elevated fasting blood glucose levels. Males (13.9%) had slightly higher impaired fasting blood glucose levels (110-125 mg/dL) than females (11.8%).11
- Cardiovascular diseases - More than a third (40.7%) of the Filipino elderly population had pre-hypertension while 35.0% had hypertension. The average systolic and diastolic blood pressure among seniors (60 years and above) was 131.6 and 77.8 mmHg, respectively. These readings fall within the category of pre-hypertension blood pressure. Elderly males had higher mean blood pressure readings of 132.5/78.8 mmHg compared to 130.9/77.1 mmHg in females.11
- Constipation - Among the elderly aged 65 years and above, 26% of women and 16% of men are constipated. In individuals 84 years of age and older, this percentage rises to 34% for women and 26% for males while the prevalence for patients in long-term care facilities might reach 80%.12
- Bone and joints disorders - Two of out ten elderly (21%) aged 60 years and above had arthritis while 1 out of 10 (1.2%) had osteoarthritis, according to data from the National Nutrition Survey in 2013.13 The same report revealed that osteoporosis also affected 0.1% and 0.7% of adult Filipinos aged 60 to 69 and over the age of 70, respectively. In addition, it was estimated that by 2050, the incidence of hip fractures will rise by 310% among men and 240% among women.14
- Micronutrient deficiency - Based on the results of the Philippine Expanded National Nutrition Survey (ENNS) [2018], 20.2% of elderly were anemic, 47% have iodine deficiency, and 1.1% had low serum retinol levels.11
- Malnutrition - Also based on the ENNS (2018), 29.2% aged 60 and above had chronic energy deficiency while 57.1% were overweight/obese. Around 9.1% of elderly also had high waist circumference (≥ 102 cm for males and ≥ 88 cm for females) while 31.2% had a high waist-hip ratio.11
Our Answer: Tips On How To Maintain Good Nutrition For the Elderly
To cap it off, check out this checklist for the elderly’s road to a healthy life through good nutrition:
- Serve healthy and tasty meals on time: To whet the weakened taste buds, choose rainbow colors through fruits and veggies with high vitamin content but low in fat. It is also essential to serve it on time to promote appetite.
- Serve meals in smaller portions but several times a day: The elderly have lower basal metabolism so smaller servings allow the body time to absorb the food.
Challenged to think of a whole day menu for the elderly? Here’s a sample menu for inspiration!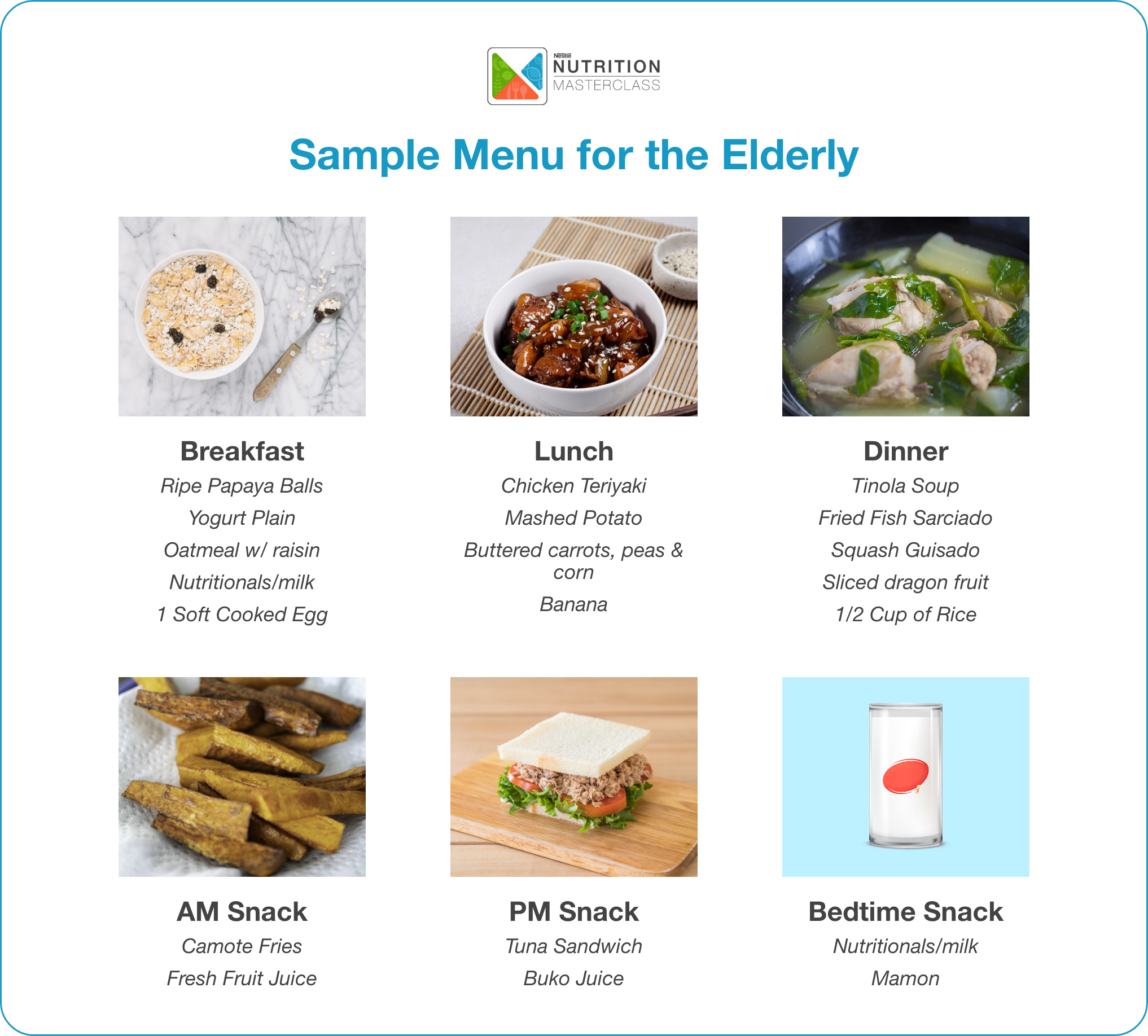
Make the meals more nutrient dense with extra calories: This is for the inclusion of nutritional supplementation and apart from extra calories, here are essentials that must be incorporated into the diet:

- Make mealtime enjoyable and socially fun: Invite family and friends to increase appetite since the elderly are prone to loneliness and to an extent, even mental health issues.
- Engage in regular physical activities: Activities such as brisk walking and social dancing should be incorporated into the routine for overall wellness.
Conclusion
Good nutrition is very important as we go through life, more so as we age. Aging is linked to physiological changes like altered hormonal responses, decreased metabolic rate, slower gastric emptying time, and altered sense of smell and taste, which can contribute to nutrient deficiencies and malnutrition. Malnutrition can contribute largely to the progressive decline in health, reduced physical and cognitive function, and with limited social interaction, isolation can result to depression and decreased quality of life, resulting to an increased risk of mortality.
These factors render elderly feeding to be very challenging. But even with the numerous problems, hope is not completely lost as healthy meals and healthy preparations are countless and easily available everywhere. With the effort to create attractive and appetizing dishes, the challenges set by aging are a battle to win. And this battle is one against time.
Message to RNDs
To ensure success in elderly feeding, we must consider some essentials to remember:
- Plan meals to ensure variety, balance, and moderation
- Create a budget-friendly food list
- Keep calories in mind appropriate to the needs
- Consider preparation time and ease in preparing daily meals
- Careful attention as to the consistency, temperature, and texture of foods
- Position of the elderly while feeding to prevent possible regurgitation and aspiration
Dietitians play an important role in ensuring optimal health throughout the aging process. The physiology of aging is very complicated and nutrition requirements are much more different. The dietitians help in making sure that adequate nutritional levels are maintained to prevent malnutrition and its adverse effects. Malnutrition is a “battle we must win” in all aspects of continuum care to promote quality of life and optimal health no matter the stage in life.


 Perla Sorreda - Esguerra , RND
Perla Sorreda - Esguerra , RND















No comments here yet.